KEY PERSONNEL: Dr. Fred C. Semitala (Co-PD), Dr. Nelson K. Sewankambo (Co-PD), Dr. Isaac Kimera (Training Coordinator), Shardrack Wanyina (eLearning Coordinator/M&E), Martin Muddu (Advisor HIV Care and treatment), Moses Adengo (Finance Administrator)
KEY PERSONNEL: Dr. Fred C. Semitala (Co-PD), Dr. Nelson K. Sewankambo (Co-PD), Dr. Isaac Kimera (Training Coordinator), Shardrack Wanyina (eLearning Coordinator/M&E), Martin Muddu (Advisor HIV Care and treatment), Moses Adengo (Finance Administrator)
PROJECT TITLE: Education for Interprofessional HIV Service Delivery in Uganda (EIPHIV-U)
PROJECT YEAR 1 RECAP: The goal of year 1 was to equip Uganda’s next generation of HIV health care providers as interprofessional practitioners, with enhanced knowledge and skills that are aligned with PEPFAR Country Operational Plan (COP) and Uganda Ministry of Health (MoH) priorities, upholding the principles of continuous quality improvement (CQI) and continuous learning to provide high quality team-based care for PLHIV.
To meet this goal, a collaborative interprofessional committee of HIV practitioners was established to train and mentor health practitioners in HIV care at Makerere University and four additional collaborating institutions. The STRIPE HIV modules were harmonized with existing Uganda MOH training content and delivered to newly qualified health professionals at all collaborating institutions. In all, 110 facilitators led 13 workshops, providing training to 655 learners (212 pre-service, 443 post-graduate).
PROJECT YEAR 2 SUMMARY: In the context of COVID-19, while still aligning with the Uganda national HIV prevention and response priorities, the year 2 goal was to enhance interprofessional, quality HIV care by implementing differentiated training modalities using online and digital training resources for the pre-service and in-service health care providers. To this end, EIPHIV-U participated in both the eLearning start-up and scale-up phases of STRIPE HIV in year 2, benefitting both (1) Ugandan learners, and (2) participants across the STRIPE HIV network:
- In the start-up phase, EIPHIV-U developed best practices for eLearning and created their own learning management system (LMS), which they continued to use for their learners in the scale-up phase. Additionally, in the scale-up phase, the project team extended mentorship to health facilities with EIPHIV-U alumni and innovated a multi-layer approach involving training, mentorship, and interprofessional QI projects to health professionals at facilities with suboptimal performance on HIV indicators. EIPHIV-U’s outcomes, identified through a rigorous evaluation, indicate the project strategies enhanced performance at both the facility output and patient outcome levels.
- Through testing and development efforts in the start-up phase and training and capacity building efforts in the scale-up phase, the project team also contributed to the build and uptake of the STRIPE-wide LMS (owned and operated by AFREhealth).
MAIN ACCOMPLISHMENTS
- The team supported the build of the new AFREhealth-owned LMS and its use for STRIPE HIV training by (1) providing technical support and feedback to AFREhealth, (2) Moodle training to 105 STRIPE HIV facilitators, and (3) piloting a mini-STRIPE HIV course to test functionality and suggest improvements prior to scaling STRIPE HIV eLearning across all partners.
- An EIPHIV-U LMS was established and utilized to train 496 learners (110% of training target) across the five collaborating institutions. Over 91% of 128 sampled trainees reported improvement and application of knowledge obtained from training.
- Twenty-five online case-based mentorship sessions were conducted with facilities that had interprofessional learners complete the EIPHIV-U course; 185 learners participated in all. The mentorships consolidated the lessons from the trainings and further enhanced interprofessional collaboration and discussions within the health facility teams, thus empowering the trainees to identify existing gaps in health service delivery and address them as an interprofessional team.
- As a special initiative to improve HIV patient outcomes at PEPFAR-supported sites, 55 HIV health care providers from five health facilities with suboptimal PEPFAR performance were targeted to participate in EIPHIV-U module training and case-based mentorships. Four of the five facilities in turn pursued interprofessional QI projects; after only 6 weeks, improvements were seen at all four facilities (Figure 1). These results indicate an interprofessional approach to HIV care improves ART adherence and viral load suppression.
Figure 1. Quality improvement projects at the targeted health facilities in line with the base indicators
|
Health Facility |
Quality Improvement project |
Baseline |
After six weeks |
|
Health Facility A |
To improve the 12 month retention of clients initiated on PrEP from 4% to 60% by January 2022 |
4% |
80% |
|
Health Facility B |
To improve the VL coverage of KPs active in care from 50% to 95% by 27th November 2021 |
50% |
94% |
|
Health Facility C |
To improve VL suppression from 82% to 95% by March 2021 |
80% |
96% |
|
To improve the VL coverage from 82% to 95% for eligible clients by 27th October 2021 |
82% |
98% |
|
|
Health Facility D |
To improve percentage annual retention of KPs from 63% to 95% by December 2021 |
63% |
85% |
KPs – Key Populations, VL – Viral load, PrEP – Pre- Exposure Prophylaxis *Green: Satisfactory performance, Yellow: Needs improvement, Red: Unsatisfactory
- The EIPHIV-U project presented findings in two abstracts at the 2021 AFREhealth Symposium and was featured in four articles in three Uganda news outlets, including the two leading national newspapers. The latter contributed to increased demand for training and broader dissemination of results.
- Over 99% of 128 surveyed post-graduate learners reported the STRIPE HIV modules to be relevant to improving HIV outcomes in their facilities. Participants specifically identified the emphasis on quality improvement (and the End of Life Care module) to fulfill a gap in the medical school curriculum.
- A mixed-methods evaluation was completed by an external team to evaluate project design, implementation, achievements, lessons learned, and recommended best practices. Select results are presented in this profile and more information is available upon request.
CHALLENGES AND SOLUTIONS
Adapting to accelerate improvements in provider practice and patient outcomes
- After observing targeting pre-service health workers was not translating into desired improvements in HIV outcomes, EIPHIV-U switched to only training in-service health workers directly involved in HIV service delivery.
- Despite learners’ expressed value and preference for the interprofessional approach, a field study on learner perspectives signaled some resistance to the approach in practice. During training, some learners reported difficulty in learning alongside others of different professions or felt some health workers acted superior to others in different professions, although these perspectives tapered in later weeks of training. Back in the workplace, alumni reported the challenge of changing the “traditional” of way of HIV service delivery in the facility. Additionally, participants reported pursuing mechanism to better facilitate interprofessional collaboration in their workplace (see Broader Impact). This speaks to how strong health professional silos are, and even more, the important role STRIPE HIV plays to flatten hierarchies in health care.
- Related to the above two challenges, EIPHIV-U also shifted to training health workers from the same facility together, and found doing so resulted in more and quicker change in HIV outcomes in facilities where at least three workers were trained from the same facility as opposed to other facilities represented by just one health worker.
Online learning
- After experiencing an initial learner dropout rate of 25% in the first training cohort (May 2021) innovations were implemented to achieve 93% course completion (7% dropout) by the third training cohort (July 2021), with some institutions achieving nearly 100% completion (0% dropout). Innovations included phoning the applicants to explain the course and expectations prior to the training; providing weekly internet data instead of monthly; sharing daily completion reports with facilitators to follow up on learners that were lagging behind; and developing LMS guidance materials.
- Naturally, online learning creates challenges of keeping learners engaged to achieve the same level of learning that takes place face-to-face. Diversifying training approaches through Zoom discussions, WhatsApp groups, and LMS forums and spreading out these approaches over multiple days helped to reiterate and thus successfully convey key points.
- A challenge remains that online training is only available to those with internet access. The EIPHIV-U team would like to reach health workers in lower facilities, including village health teams working with HIV clinics. A solution to test in the future is offer blended learning to ensure equitable access to the course.
TRAINING PARTNERS
Pre-service learners were recruited from the universities/colleges listed below. The five EIPHIV-U collaborating institutions are indicated by an asterisk (*).
- Makerere University*
- Busitema University*
- Clarke International University*
- Kabale University*
- Lira University
- Nsambya Hospital Training School*
- Kampala International University
- Mbarara University of Science and technology
PARTICIPATING CINICAL SITES
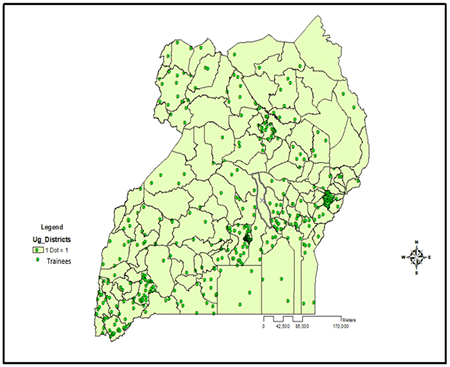
EIPHIV-U completed nation-wide recruitment of working health professionals and received over 600 applications. The selected post-graduate learners worked in 208 health facilities, with 189 (91%) of those facilities receiving PEPFAR support (Figure 2).
Figure 2. A dot-density map showing the distribution of EIPHIV-U year 2 trainees across Uganda
IMPLEMENTATION
- # Training cohorts: 3
- # Facilitators: 35
|
Profession |
Years of experience |
Gender |
Teaching experience |
||||
|
Medical |
23 |
0-5 years |
7 |
Male |
16 |
HIV educator |
35 |
|
Nursing/Midwifery |
7 |
6-10 years |
13 |
Female |
19 |
Non-HIV educator |
0 |
|
Pharmacy |
1 |
> 11 years |
15 |
Other |
|||
|
Laboratory |
2 |
||||||
|
Other |
2 |
||||||
- # Learners: 496
|
Medical |
Nursing/Midwifery |
Pharmacy |
Laboratory |
Other |
Total |
|
|
Preservice |
9 |
3 |
1 |
4 |
0 |
17 |
|
Postgraduate < 12 months |
66 |
64 |
1 |
4 |
5 |
140 |
|
Postgraduate > 12 months |
126 |
147 |
3 |
44 |
19 |
339 |
|
TOTAL |
201 |
214 |
05 |
52 |
24 |
496 |
|
Gender |
|
|
Male |
278 |
|
Female |
218 |
|
TOTAL |
496 |
INNOVATING HIV TRAINING DURING COVID-19: The transition to online learning enabled participation by health workers that could not have been easily reached with face-to-face training, including health workers located on the remote islands of Lake Victoria. As a result of the diversity of facilities represented in the online trainings, there was greater knowledge-sharing among health workers with different backgrounds and experiences.
BROADER IMPACT: Various advisory board, technical committee, and dissemination meetings were held to promote the EIPHIV-U model to Makerere University, Ministry of Health, and PEPFAR/Uganda leadership. Across the board, stakeholders agreed the “targeted training” approach is a critical link to addressing the remaining gaps in HIV service delivery and sustaining PEPFAR gains in Uganda. They also expressed value for the emphasis on teamwork, patient-centered care and collaborative decision-making, as well as its aim towards sustainability through working with health facility leadership and implementing partners.
There are early signs of health system impact and sustainability:
- Over 55% of 128 sampled trainees reported an interprofessional approach has been adopted at the health facility where they work
- Standard operating procedures on interprofessional practice have been developed from EIPHIV-U training materials at supported health facilities
- One partner institution (Busitema University School of Medicine) has now included interprofessional learning and practice in their curriculum for training undergraduates.
- The Infectious Disease Institute (a PEPFAR implementing partner) plans to incorporate the approach to improve HIV care performance in other facilities beyond those supported by EIPHIV-U.
The EIPHIV-U experience in year two produced many best practices that STRIPE HIV would like to adopt in future project years, namely: (1) the multilayered approach of training, mentorship and QI projects, (2) recruiting learners by groups from the same health facility so that they return to a peer environment that values and thus maintains a culture of interprofessional collaborative practice, and (3) targeting learners from HIV facilities with suboptimal HIV patient outcomes.
IMPACT VIGNETTES
Increased reach and flexibility with the online training
- Providing the online training has enabled some of us in up country health facilities to receive mentorships, unlike the face-to-face training when we were left out; I am grateful. - Doctor learner, Adjumani hospital (445 Kilometers from Kampala)
- Transitioning to the online course has provided a lot of flexibility and leverage, especially during the Covid-19 pandemic times that would have made the face-to-face trainings with multiple learners impractical. The flexibility of the online training, has allowed busy in-service health professionals to successfully complete the course. Additionally, we have reached more trainees from remote facilities that we previously could not, who have equally benefited from the course as their fellow health workers in urban facilities.”- Facilitator, Clarke International University.
- We selected participants for the online training from different health facilities, with different backgrounds and experiences. This has enabled sharing knowledge and best practices between the learners, like during a follow-up call, a previous trainee informed of how he learnt of a practice of assigning unsuppressed clients between the healthcare team for accountability - from a fellow learner during the training - and this initiative, has not only improved monitoring of unsuppressed clients who were getting lost to follow up, but also enhanced interprofessional practice at their health facility, since the patients are assigned to all health workers regardless of the cadre. – Facilitator, Busitema University School of Medicine
Interprofessional Collaboration
- One of the junior doctors at Mbale RRH who completed the training, has greatly appreciated the concept of IPE/IPP and has now embarked on improving IPP on his ward. Most recently, he reported to have made a presentation on interprofessional practice to the ward team where he works. The idea was embraced, and now during ward rounds he ensures that the nurses, pharmacist, counselor and doctors do a ward round together and discuss issues jointly. He has noticed some improvements in timeliness of implementation of decisions made during ward rounds. – Facilitator, Busitema University School of Medicine).
- Working as an interprofessional team has made the greatest difference. Normally, every health worker is focused on completing their tasks. However, the training has enabled us to learn together, and after, collaborate to identify root causes of the low performance on the indicators and collectively come up with solutions. We will use the same approach to address other challenging indicators. – Nurse learner, Kasozi HC3
- The online course has improved engagement among health professionals because most of the health workers from our clinic were enrolled to the course at the same time, this made the Zoom sessions very interactive and the role plays were excellent, we chose to have these sessions in the evening when much of the clinic work is done- a win for us and the patients. – Clinical officer, Mbarara Regional Referral hospital ISS clinic.
Quality Improvement
- l have learnt communication skills especially when interacting with difficult clients, and how to apply quality improvement techniques to identify gaps in service delivery, which is essential for improving care at our facility. – Nurse learner, Kisugu HC3
- I have realized that as a Laboratory Technician, I have an important role to play in an interprofessional team for quality service delivery, just as any other professionals. If I do not deliver laboratory results on time, then I will cause a bottleneck. Thank you for this training. – Lab Technician learner, Mbale Regional Referral Hospital